We are winging it home from San Juan, Puerto Rico, after the American College of Medical Toxicology Annual Scientific Meeting. I am lucky enough to be sitting next to Dr. Christina Hernon, whose presentation, “Twisted: Understanding the Neural Pathways of Addiction” shined a light on an area of increasing importance in medical toxicology.
If you’ve never met Dr. Hernon, one of her superpowers is distilling complex ideas into comprehensible bits. I had the chance to ask her about her favorite take-home messages from the lecture.
1. We are finally putting the bio- into the biopsychosocial model of addiction.
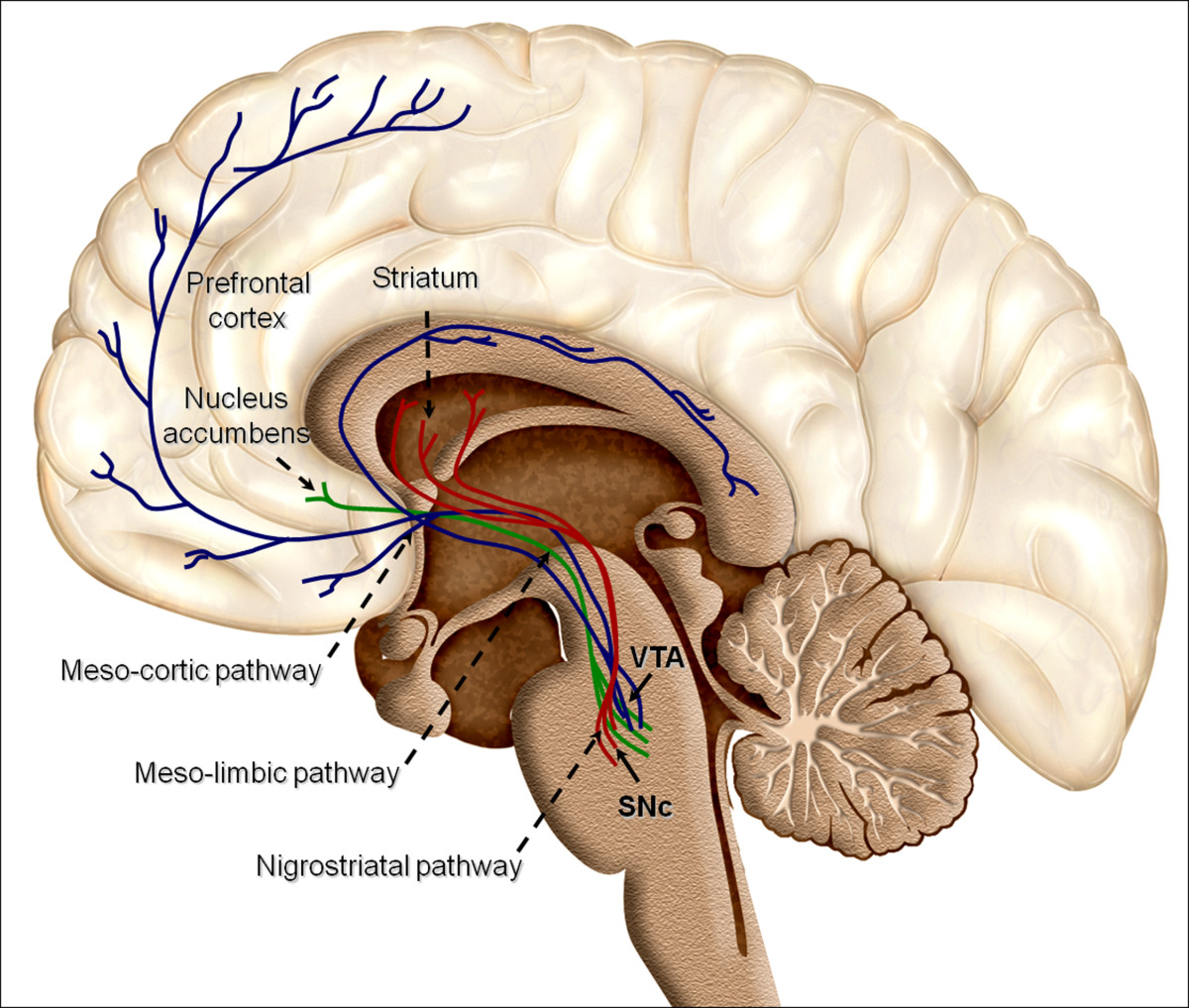
Our understanding of addiction is evolving rapidly. Historically, laypeople, family members, and even doctors pointed the finger at the addicted patient, assuming some sort of social flaw, moral failing, or lack of willpower drove the addiction and prevented recovery. But by understanding the biology underlying addiction (the pathways, structures, neurotransmitters, transporters, etc.) that are ultimately overtaken or hijacked in addiction, the more we can respect the drive towards addiction and the complexity of recovery.
2. First exposures are critically important.
A recent MMWR article indicated that a 10-day opioid prescription leads to a 1 in 5 chance that the patient will still be on an opioid one year later. What impressed me the most from the emergency physician point-of-view is that the same article had a graph showing that even a 1-day prescription for an opioid leads to a 6% chance that the patient is still on an opioid at one year. Here’s an example drawing from these data. If an emergency physician writes 5 opioid prescriptions per week for a 1-day supply, then in one year, 15.6 of that physician’s patients will still be taking opioids. We must be mindful of the long-term impact of opioid prescriptions, including those of short duration.
3. Humans are driven towards homeostasis.
To find homeostasis, we balance sensory input of two main categories. The first is exteroception, or sensing the physical world. Think proprioception or discriminatory touch. The second is interoception, which includes thirst, hunger, temperature, pain, itch, and tickle, among others. Some of the sensations of withdrawal overlap with these interoceptive inputs. As a result, the drive for homeostasis effectively includes a drive to alleviate the symptoms of withdrawal that rivals the drive to eliminate feelings of thirst, hunger, and pain.
Understanding the biology of addiction is key to destroying any lingering shame or stigma faced by our patients with addiction.
Authors: Dr. Christina Hernon and Dr. Kavita Babu